St Vincent’s Lismore is committed to ensuring it is providing high quality and safe care to our patients and has built a strong culture of continuous quality improvement. In order to achieve this, St Vincent’s Lismore recognises the need to regularly gather and monitor patient experience and clinical and quality outcome data in order to:
- Identify and understand our own performance;
- Be open and honest about the quality and performance of the services we provide;
- Proactively use the data and outcome measures to evaluate and improve our service;
- Incorporate our patients and community in the evaluation of our services and use their input to improve our service delivery;
- Provide our patients and community with information in order for them to make an informed decision about their hospital of choice.
St Vincent’s Lismore’s clinical governance system ensures a wide range of clinical quality areas are monitored at all levels to ensure performance is to standard (as a minimum), to identify new service opportunities and ensure continuous quality improvement is a standard part of clinical quality and patient safety.
In addition to St Vincent’s Lismore internal clinical governance systems, we participate in the Australian Council for Healthcare Standards (ACHS) Clinical Indicators Program. This program encompasses a range of measures focusing on the outcomes of our patient care.
The ACHS provides us with a report on our individual performance, along with a comparison against each individual measure with relevant industry benchmarks.
View our results:
- Blood Transfusions
- Falls
- Hand Hygiene
- Healthcare Associated Infections
- Medication Safety
- Pressure Injuries
- Rapid Response
- Rehabilitation – Functional Independence Measure
- Unplanned Readmissions within 28 Days
- Unplanned Returns to Theatre
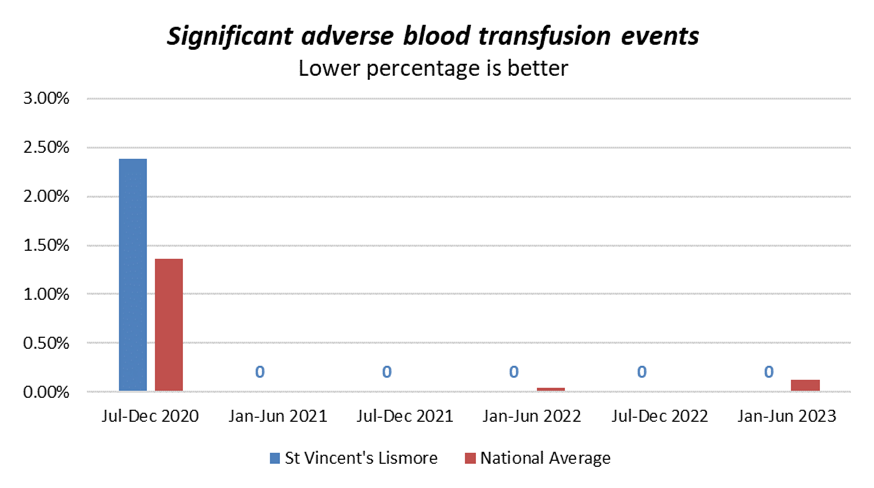
BLOOD TRANSFUSIONS
As part of your hospital admission, you may require a blood transfusion, which is a procedure where you receive blood through an intravenous cannula in your vein. Blood transfusions may be necessary for a number of reasons, for example: if you have a surgical procedure, you are anaemic or if your body is not producing sufficient blood cells. Blood transfusions can be a lifesaving measure, but are not without some risk and therefore are only prescribed after a doctor has deemed it necessary. Sometimes an adverse reaction to a blood transfusion can occur and is treated immediately. Blood transfusion administration and management are governed by the Australian Commission on Safety and Quality in Health Care Standard for Blood and Blood Products. The hospital consistently has zero significant adverse blood transfusion events.
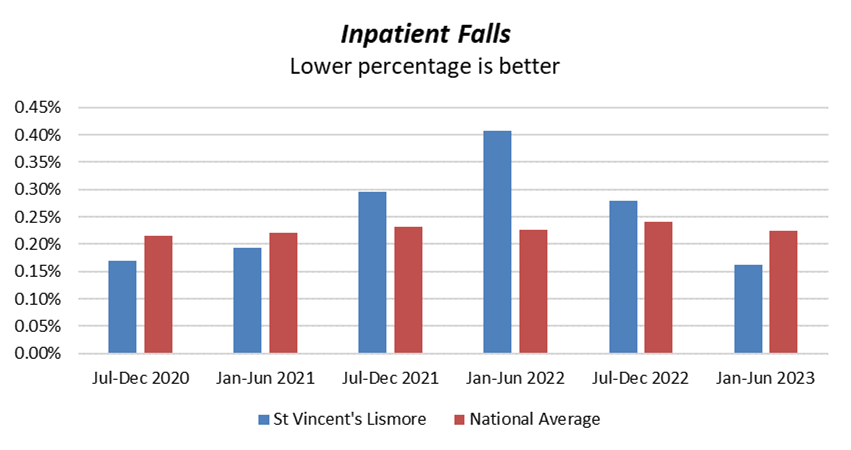
FALLS
The risk of falls increases according to age with data suggesting that one third of people over the age of 65 years have one or more falls a year.
Whilst falls can occur at all ages, the frequency and severity of falls-related injuries increases significantly with age. These injuries can include minor skin abrasions, joint dislocation, fractures and head injuries. These injuries may result in hospitalisation or an increased length of stay in hospital.
The risk of falling can greatly increase when admitted to hospital due to a range of factors including illness and unsteadiness, adapting to a new environment, the introduction of new medications and walking in unsafe footwear or slippers.
In 2017, St Vincent’s Lismore increased the focus on falls prevention by joining a National Falls Prevention Advisory Group. Our hospital uses a number of strategies to prevent falls. We also participate in the National “April Falls Day”.
HAND HYGIENE
Hand hygiene is the single most important factor in reducing hospital acquired infections and has been nominated as a priority area by the Australian Commission on Safety and Quality in Health Care (ACSQHC).
St Vincent’s Lismore participates in the national hand hygiene strategy through Hand Hygiene Australia (HHA). HHA has established a consistent best practice application for hand hygiene, referred to as the ‘five moments for hand hygiene’ that is: before touching a patient, before a procedure, after a procedure, after touching a patient and after touching a patient’s environment.
Visitors to this hospital are encouraged through appropriate signage to use antiseptic hand rub located throughout the hospital.
Hand Hygiene Compliance
St Vincent’s Lismore participates in Hand Hygiene Compliance auditing through Hand Hygiene Australia. This auditing program is based on trained hand hygiene auditors undertaking observational audits of staff compliance three times per year with the application of the ‘five moments of hand hygiene’.
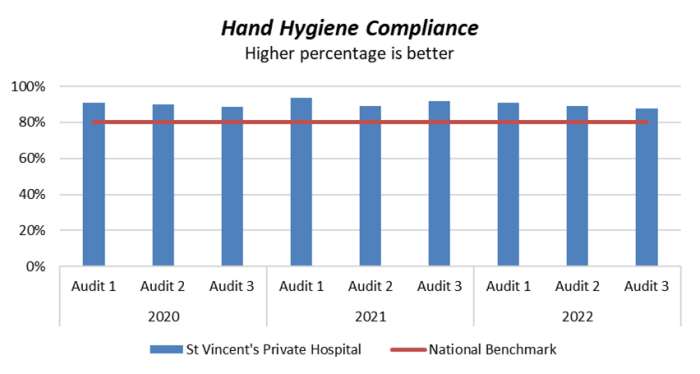
The above graph shows St Vincent’s Lismore’s percentage of compliance of observed correct moments of hand washing. The Hand Hygiene Australia benchmark is currently 80%, therefore anything higher than this is acceptable – the higher percentage the better.
These results are submitted to Hand Hygiene Australia for inclusion in a national database and are publicised on the MyHospitals website.
For further information visit the Hand Hygiene Australia website
HEALTHCARE ASSOCIATED INFECTIONS
At St Vincent’s Lismore, we aim to minimise the risk of infection to patients, staff and visitors who come to our facility. This hospital has a number of programs in place to detect and prevent infections that are common within health care facilities.
One of the most effective means to prevent infection spreading amongst patients is for all health professionals to wash their hands.
Staphylococcus Aureus Bacteraemia (SAB)
In addition to Hand Hygiene data, St Vincent’s Lismore provides data on the number of cases of SAB (per 10,000 bed days of patient care) for reporting through Hand Hygiene Australia (HHA).
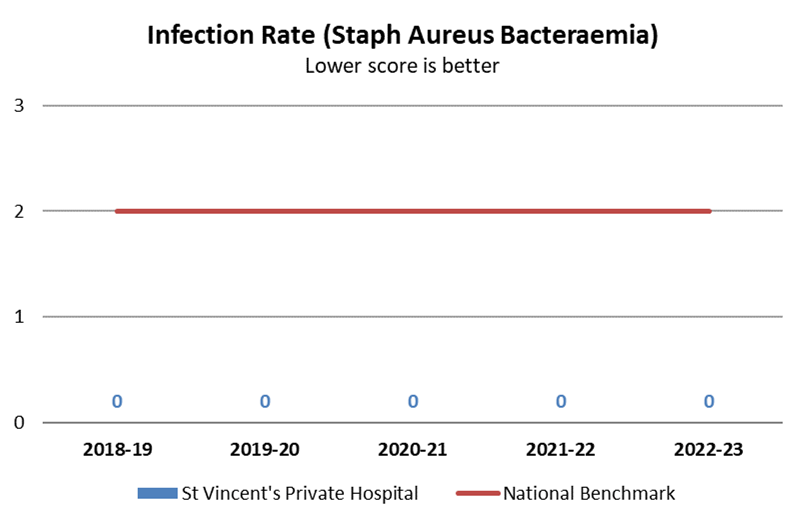
The above graph shows St Vincent’s Lismore’s occurrence of healthcare associated staphylococcus aureus bacteraemia (SAB). The current national benchmark is two (2) cases per 10,000 days of patient care. A lower rate is better. The hospital consistently has zero cases of SAB.
These results are submitted for publication on the MyHospitals website.
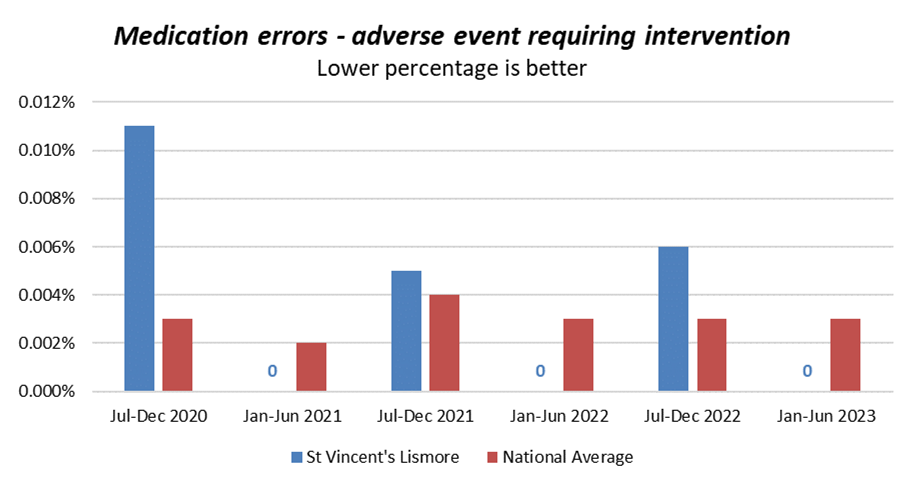
MEDICATION SAFETY
Medicines are commonly used to treat a variety of conditions in the healthcare setting and therefore it is important to measure the risk of errors. St Vincent’s Lismore is continually reviewing and implementing a range of medication safety strategies to further improve performance in this area.
The Australian Commission on Safety and Quality in Health Care has introduced a number of safety initiatives for medication administration and reconciliation and St Vincent’s has adopted many of these strategies. This includes the National Inpatient Medication Chart which standardises the documentation on how medicines are prescribed and ordered. Adoption of the User-Applied Labelling of Injectable Medicines recommendations has assisted in preventing medication errors related to the wrong route, dose or medication being administered.
In addition, we have medication administration policies and processes in place which have been developed using best practice principles.
St Vincent’s Lismore takes all medication errors very seriously. We encourage staff to report all errors no matter how minor they may seem. All medication incidents are investigated and actioned. Any serious medication incidents are investigated thoroughly.
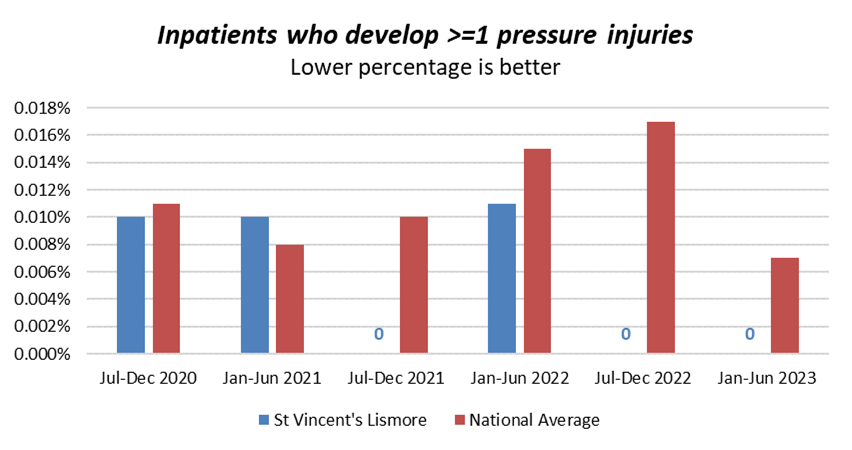
PRESSURE INJURIES
Pressure injuries are wounds which form as a result of prolonged pressure to an area of skin. Pressure injuries are recognised worldwide as a common cause of harm to patients and can cause significant pain and discomfort which may result in slower recovery for the patient.
St Vincent’s Lismore is well equipped with the latest equipment to assist staff to prevent these injuries from occurring. Patients are risk-assessed on admission using an evidence-based tool. Staff follow a care plan which is targeted to minimising a patient’s risk of developing a pressure injury for those patients assessed as high risk. This includes inspecting the patient’s skin frequently, managing moisture, keeping the skin dry, optimising nutrition and hydration and moving the patient frequently or using special pressure relieving mattresses when needed. Referral to our specialist wound nurse is mandatory for all patients with an existing pressure injury.
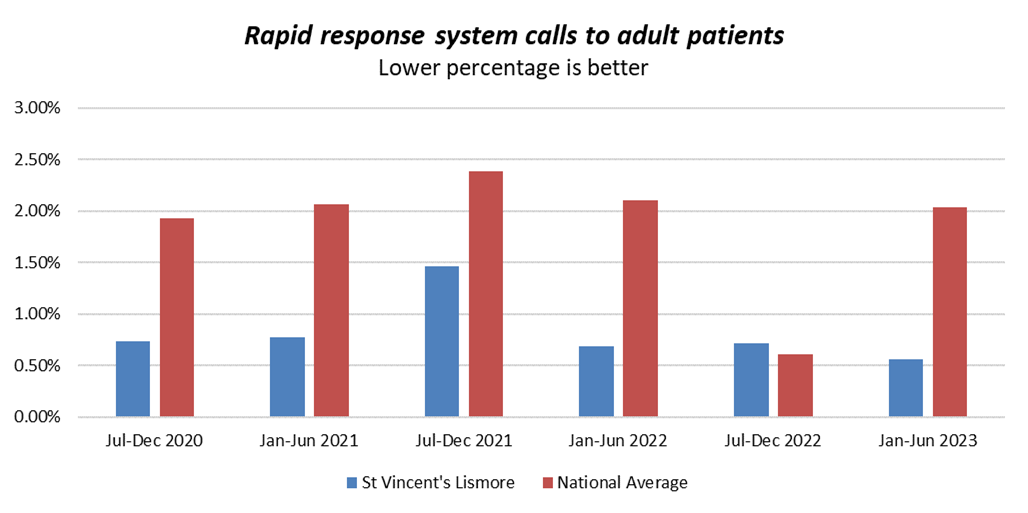
RAPID RESPONSE
Our organisation-wide systems support and promote detection and recognition of acute deterioration, and the response to patients whose condition acutely deteriorates. These systems are consistent with the National Consensus Statement: Essential elements for recognising and responding to acute physiological deterioration.
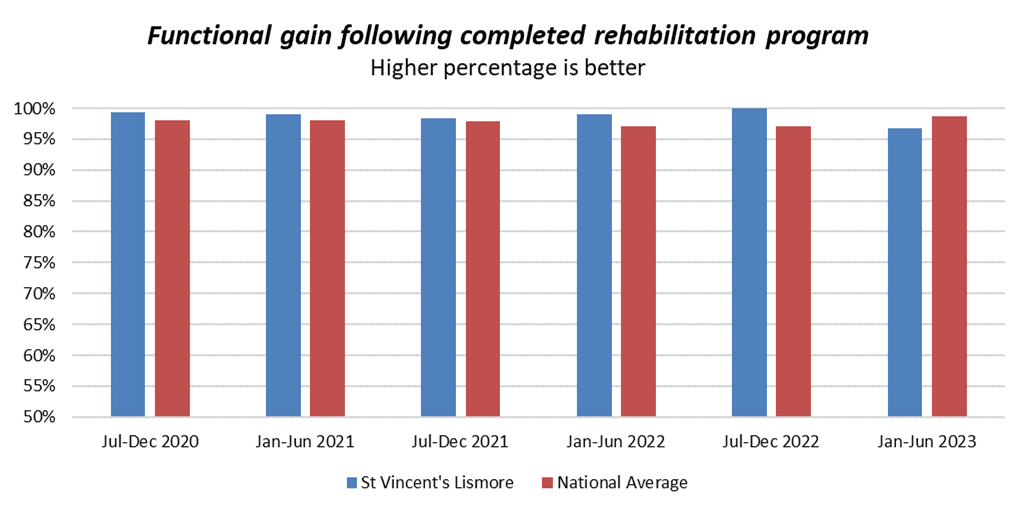
REHABILITATION – FUNCTIONAL INDEPENDENCE MEASURE
Rehabilitation programs aim to enable the highest level of independence (physically, psychologically and socially) to people with loss of function or ability due to injury or disease. At the time of admission into the rehabilitation program the patient has a Functional Independence Measure (FIM) rating conducted by a qualified member of the rehabilitation team. The FIM is redone during and at the end of the program to determine the patient’s functional improvement and therefore the level of independence gained in activities of daily living. Progress in the areas of social interaction and psychological wellbeing is also measured. The FIM is the industry standardised functional assessment tool that is used by our rehabilitation facility to measure this information. A higher score indicates that the patient has achieved a higher level of improvement in all the areas being measured. We have achieved higher than industry average scores for functional improvement.
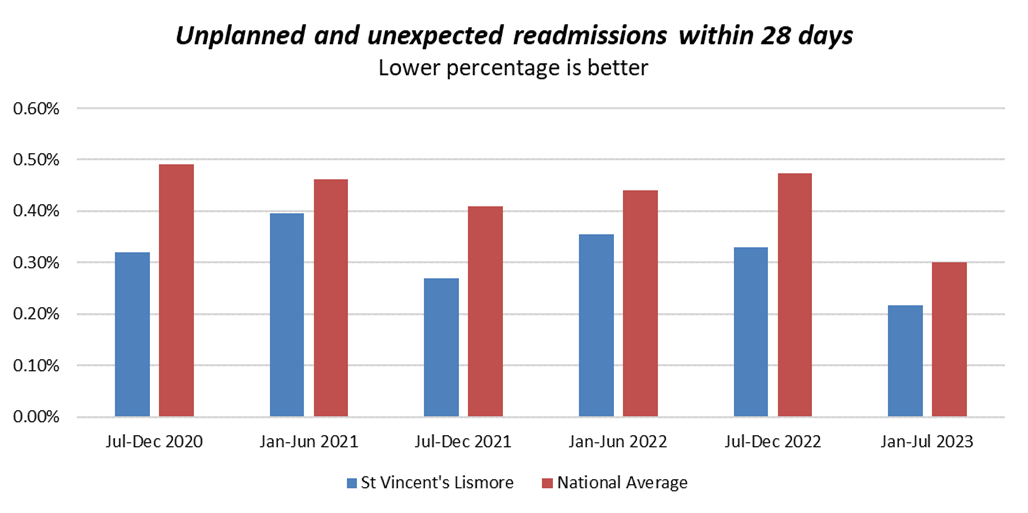
UNPLANNED READMISSIONS WITHIN 28 DAYS
Our hospital reviews patients who have an unplanned readmission to hospital following discharge. Monitoring of this information is very important as it provides an indication of the effectiveness of our discharge planning processes.
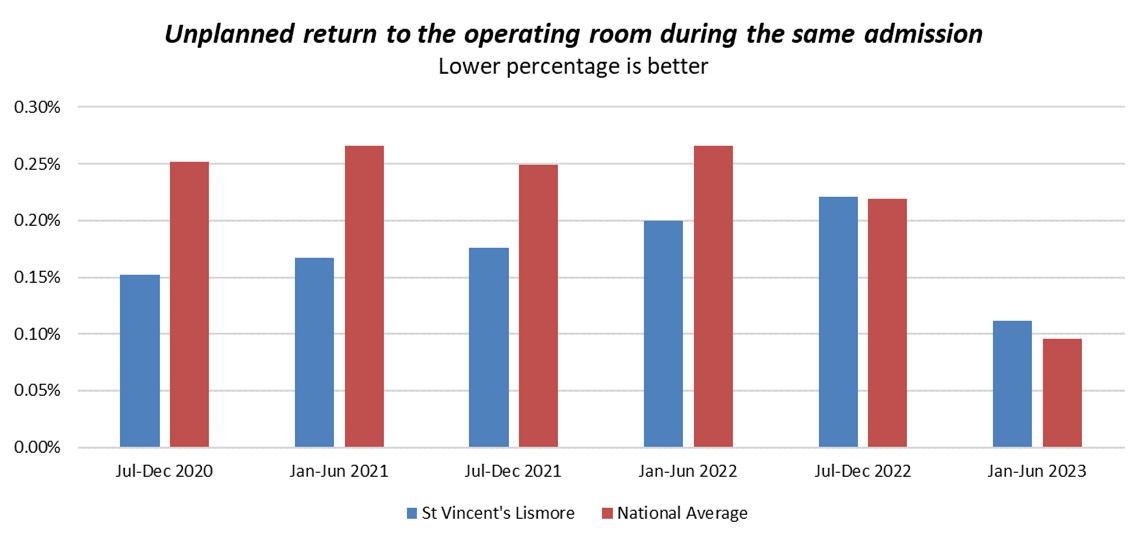
UNPLANNED RETURN TO THEATRE
St Vincent’s Lismore doctors undertake surgery in many specialty areas which range from minor procedures to more complex surgery requiring specialised care. We monitor our patient outcomes by comparing any unplanned returns to theatre to other Australian hospitals nationally. The aim is to reduce returns to theatre where possible; however there are many factors which influence these returns and sometimes these returns may save a life.
Unplanned returns to the operating theatre are frequently due to complications, for example to treat bleeding or other problems occurring early after an operation. Some complications following complex surgery are to be expected due to patients’ pre-existing diseases or conditions and the nature of the disease or condition being treated. Our hospital monitors all returns to theatre and implements any quality measures which may be required so that our patients get the best possible outcomes following surgery.